Activated Partial Thromboplastin Time (APTT)
An activated partial thromboplastin time measures the intrinsic pathway of coagulation. It will detect abnormally low levels of activity of factors XII, XI, X, IX, VIII, V, II, and I.
The test is run on the plasma that is drawn in a tube containing sodium citrate. The sodium citrate removes calcium to prevent clotting. Plasma is mixed with 2 substances that initiate the intrinsic pathway of coagulation. The first is a phospholipid that acts as platelet factors (partial thromboplastin). The second is a substance that activates factor X. The final ingredient for coagulation to occur is calcium. The amount of time it takes for the plasma mixture to clot, after the addition of calcium, is called the activated partial thromboplastin time (APTT). This time is compared to a normal control value.
CBC: Complete Blood Count

Automated Coulter Blood Analyzer
This test is usually called CBC (Complete Blood Count) with differential (different types of white blood cells present on microscopic examination). It is a very common test that is done to find out if a person is anemic, has an infection, or may have a tendency to bleed.
Several components make up the test.
1. White Blood cells (WBC): These are cells that usually fight infection. Each laboratory has a normal range usually from 4,000 to 10,000. If this count is elevated it may indicate the presence of infection or steroid treatment. If the count is low, it is usually from medications, infections, autoimmune diseases, or blood diseases among many other causes.
Instructor's Notes:
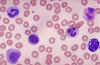
This is a normal peripheral blood smear. The large, purple cells are the white blood cells. The numerous small cells are red blood cells.
There are several types of white blood cells. Determining the percentage of the different white blood cells is called a differential. A differential is performed by manually counting 100 white blood cells from a blood smear. The percentage of each type is determined. This is important because each type of white blood cell has a different function and may be elevated or decreased in various diseases. Each type of WBC has a normal range in the laboratory. The different types of White Blood Cells are:
Neutrophils: Normal range is 60-70% of all White Blood Cells. Neutrophils may be elevated with bacterial infections, burns, stress, or inflammation. A decrease may be caused by radiation, certain drugs, vitamin B12 deficiency, or systemic lupus erythematosus.
Lymphocytes: Normal range is 20-25% of all White Blood Cells. Lymphocyte counts may be elevated in viral infections, immune diseases, and some leukemias. Low numbers may be seen in a prolonged, severe illness, during chemotherapy, and when high levels of steroids are present.
Eosinophils: Normal range is 2-4% of all White Blood Cells. Eosinophils may be elevated due to allergies, parasitic infections, autoimmune disease or adrenal insufficiency. A low eosinophil count could be caused by Cushing's syndrome, certain drugs, or stress.
Monocytes: Normal range is 3-8% of all White Blood Cells. Monocytes may be elevated from viral or fungal infections, tuberculosis, some leukemias, and other chronic diseases. Low levels are rarely seen.
Basophils: Normal range is 1/2-1% of all White Blood Cells. Elevations in basophils may be seen in allergic responses, leukemias, cancers, and hypothyroidism. A decrease may occur during pregnancy, ovulation, stress, and hyperthyroidism.
WBC's. Clockwise from left, banded neutrophil (immature form), eosinophil (note the red, granular cytoplasm), basophil (note the large, purple granules), segmented neutrophil (mature form), lymphocyte, monocyte.
2. Hemoglobin (Hgb) and Hematocrit (Hct): Hemoglobin is the iron-containing pigment of red blood cells which carries oxygen from the lungs to the tissues. The Hematocrit is the ratio (expressed as a percentage) of RBC's to the total blood volume. These tests usually indicate the presence of anemia when they are below the normal range. An elevated hemoglobin and hematocrit may occur in smokers and in polycythemia, a blood disease where there are too many red blood cells.
3. MCV ( Mean Corpuscular Volume), MCH (Mean Corpuscular Hemoglobin), MCHC (Mean Corpuscular Hemoglobin Concentration. The MCV, MCH, MCHC are calculations that reflect the size and hemoglobin content of individual red blood cells.
4. Platelet Count (PLT): Platelets are involved in clotting and prevention of bleeding. An increased platelet count is usually seen with malignancy, certain blood diseases, or rheumatoid arthritis. A low platelet count may be seen in certain blood diseases, infections, and with some medications.
Cytochemical Stains
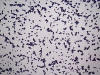
Cytochemical stains are used to identify chemical constituents within the cell. They are used primarily to differentiate the leukemias.
Evoked Potentials
An evoked potentials test records the time it takes for a sensory stimulus, such as a light flashed into the eyes, to reach the brain. The test can check the brain's response to visual, auditory, and pain stimuli. Electrodes are simply attached to the scalp, connecting the individual to an electroencephalograph (EEG), a device that records brain waves. (Rosner's Multiple Sclerosis 49.)

Factor Assays
Factor Assays test for the level of individual coagulation factors in the blood. Factor Assays are indicated after a prolonged PT or APTT (when a bleeding disorder is suspected and the patient is not undergoing anticoagulant therapy). Patient plasma is mixed with a substrate containing the factor being tested for. A PT or APTT is run depending on the factor being tested (PT for extrinsic factors, APTT for intrinsic factors). Results are compared to a standard with a known amount of the factor being tested for.
Example: Joe Black is a hemophiliac with 1% of factor VIII present in his blood. The APTT was prolonged. When the patient's plasma is mixed with a substrate containing factor VIII, the APTT is corrected, or normal. If factor IX was mixed with the patient's plasma, the APTT would still be prolonged because the missing factor had not been added. By this process of elimination, the deficient factor can be identified.
Gram Stain
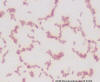
A staining procedure used to differentiate bacteria into two classifications, gram positive and gram negative. The procedure is based on the principle that gram-positive bacteria have a much thicker cell wall containing different constituents than a gram-negative cell wall.
Procedure:
1. Slides are flooded with a purple crystal violet-grams iodine complex. All cells are colored a deep blue.
2. Slides are washed with an alcohol decolorizer. Bacteria with thick cell walls retain the crystal violet stain after decolorization. Thin-walled bacteria do not retain the dye complex.
3. A pink saffron counterstain is added. All unstained elements are counterstained pink. Because the thin-walled gram-negative bacteria do not retain the original stain, they will stain pink. Thick-walled gram-positive bacteria retain the crystal violet stain and remain purple.
Gram-positive organisms are often treated with different antibiotics than gram-negative organisms. The gram stain is valuable to a physician because empiric antibiotic therapy may be started based upon the gram stain.
Immunologic Marker Studies
Certain antigens are expressed on cell lines at different stages of cell maturation. In leukemias, hematopoietic bone marrow cells stop development at a certain stage of maturation and then proliferate. By typing the antigen markers on leukemic cells, leukemias can be diagnosed and classified.
Prothrombin Time (PT)
The prothrombin time measures the extrinsic pathway of coagulation. It will detect abnormally low levels of activity of factors I, II, VII, and X.
The test is run on the plasma that is drawn in a tube containing sodium citrate. The sodium citrate removes calcium to prevent clotting. The extrinsic pathway of clotting depends on tissue factor (thromboplastin) to start the pathway and calcium. 1 part of patient plasma is mixed with rabbit lipoprotein extract that contains tissue factor. Calcium chloride is added to this mixture and the test is timed. The amount of time it takes for the plasma mixture to clot, after the addition of calcium, is called the prothrombin time. This time is compared to a normal control value.